Understanding Type 2 Diabetes Mellitus: A Comprehensive Guide
Diabetes Mellitus, commonly known as diabetes, is a chronic condition that affects how your body turns food into energy. Of its various forms, Type 2 Diabetes is the most prevalent, accounting for 90-95% of all diagnosed cases. Unlike Type 1 Diabetes, where the body doesn't produce insulin, in Type 2, the body either doesn't produce enough insulin or doesn't use insulin effectively, a condition known as insulin resistance. This leads to high blood sugar levels, which can cause a cascade of health problems if left unmanaged.
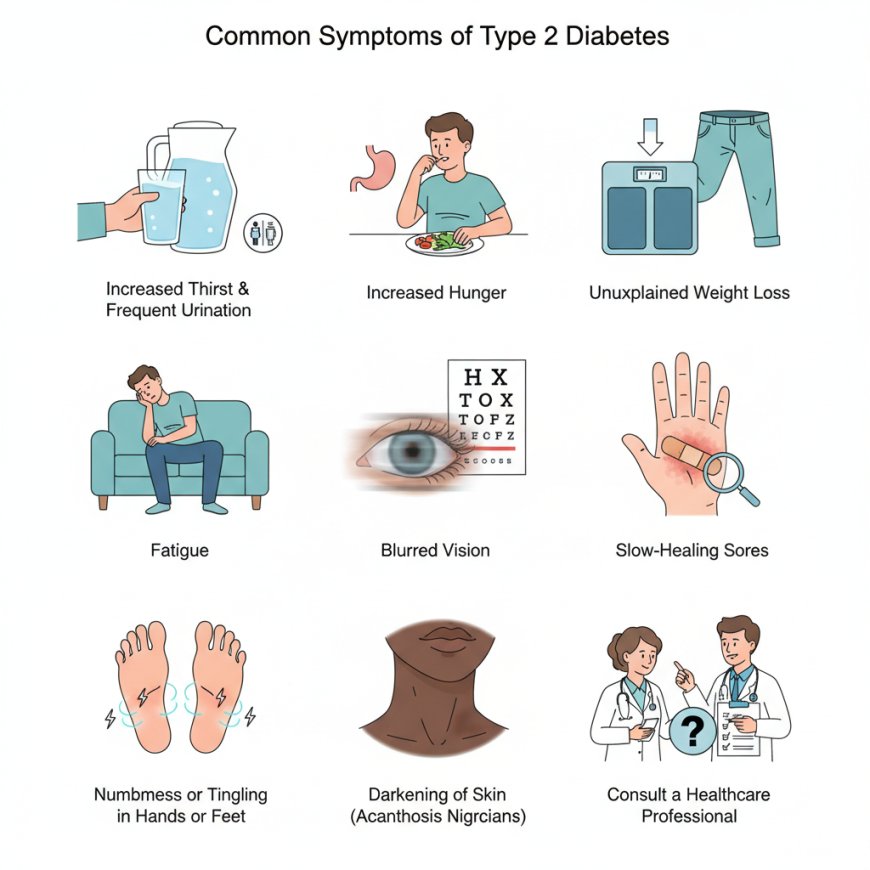
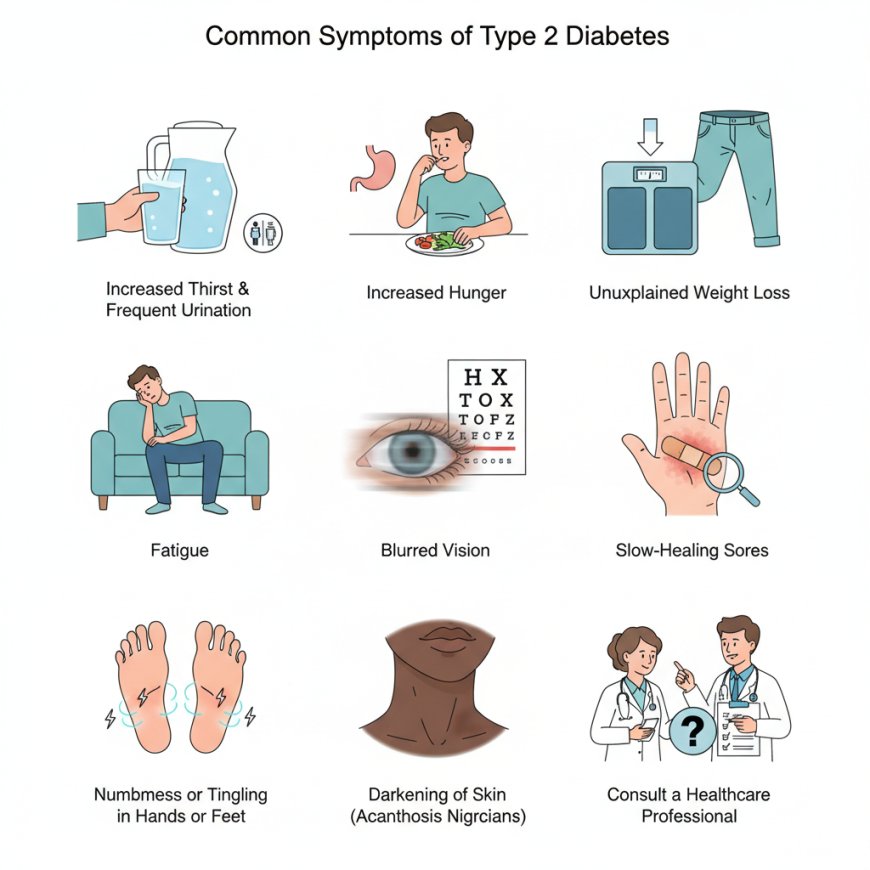
The Silent Threat: Symptoms of Type 2 Diabetes
One of the challenging aspects of Type 2 Diabetes is its often subtle onset. Many individuals may live with the condition for years without realizing it, as symptoms can be mild and develop gradually. However, it's crucial to be aware of the potential warning signs.
Common Symptoms Include:
-
Increased Thirst and Frequent Urination: When blood sugar levels are high, your kidneys try to remove the excess sugar by filtering it out of your blood. This pulls more water from your body, leading to increased urination and subsequent thirst.
-
Increased Hunger: Even after eating, individuals with Type 2 Diabetes may feel constantly hungry. This is because insulin resistance prevents glucose from entering your cells to provide energy, tricking your body into thinking it needs more fuel.
-
Unexplained Weight Loss: Despite increased hunger, some people may experience weight loss. This happens when the body starts burning fat and muscle for energy due to the inability of glucose to enter cells.
-
Fatigue: The lack of glucose entering your cells for energy can lead to persistent tiredness and a general feeling of malaise.
-
Blurred Vision: High blood sugar can affect the tiny blood vessels in your eyes, causing fluid to shift into and out of the lens, leading to temporary blurred vision.
-
Slow-Healing Sores or Frequent Infections: High blood sugar can impair your immune system and affect circulation, making it harder for your body to heal and fight off infections.
-
Numbness or Tingling in Hands or Feet: This is a symptom of nerve damage, a potential long-term complication of uncontrolled high blood sugar.
-
Darkening of Skin (Acanthosis Nigricans): Patches of darkened, velvety skin, often in the armpits, neck, and groin, can be a sign of insulin resistance.
If you experience any of these symptoms, it's essential to consult a healthcare professional for proper diagnosis and management.
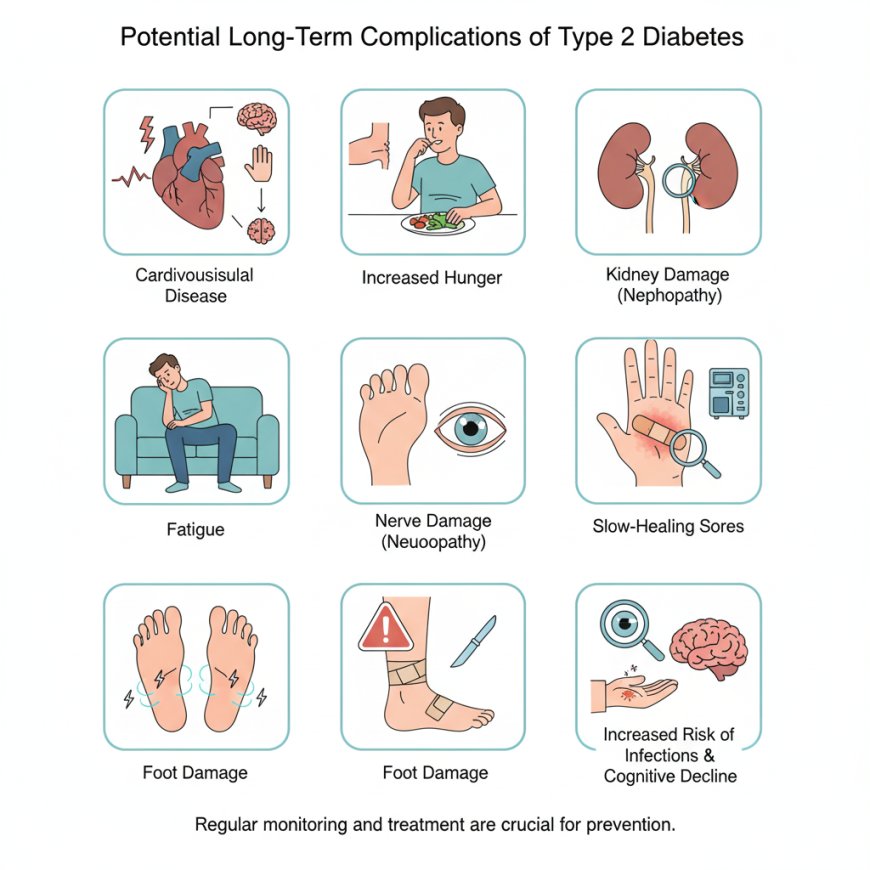
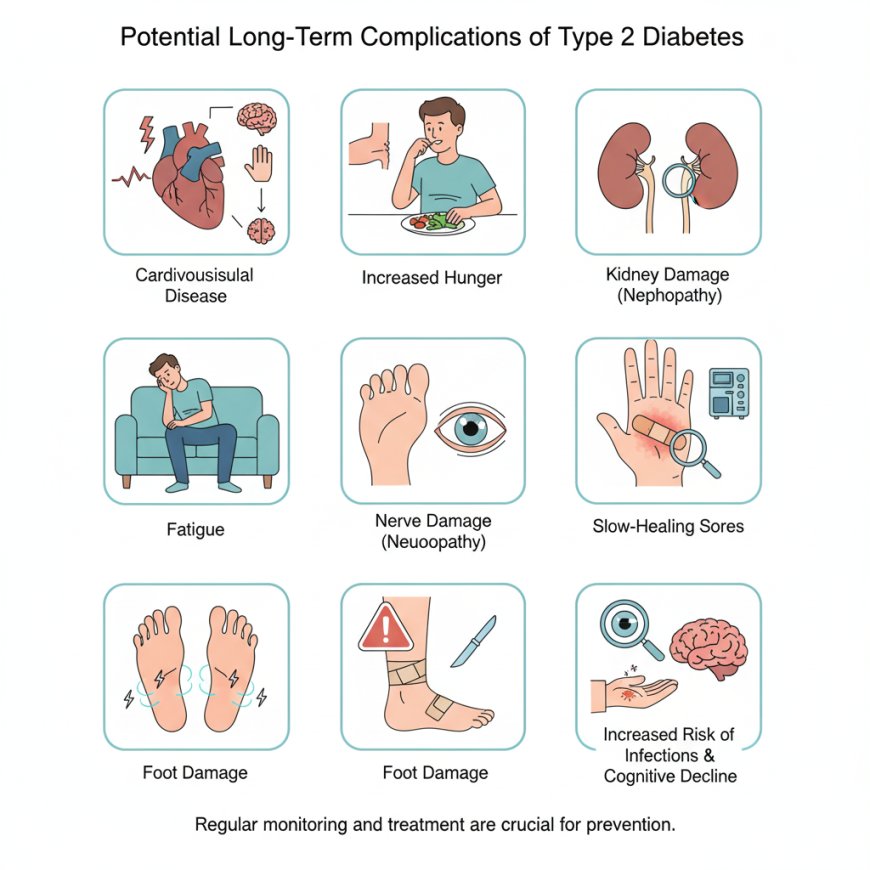
The Course of Type 2 Diabetes: Progression and Complications
Type 2 Diabetes is a progressive disease, meaning it tends to worsen over time if not effectively managed. Initially, the body may compensate for insulin resistance by producing more insulin. However, over time, the pancreas can become exhausted and produce less insulin, leading to higher blood sugar levels
Potential Long-Term Complications Include:
-
Cardiovascular Disease: Diabetes significantly increases the risk of heart attack, stroke, and other heart and blood vessel problems.
-
Nerve Damage (Neuropathy): High blood sugar can damage nerves throughout the body, leading to numbness, tingling, pain, or weakness, especially in the hands and feet.
-
Kidney Damage (Nephropathy): The kidneys' filtering system can be damaged, potentially leading to kidney failure and the need for dialysis or a kidney transplant.
-
Eye Damage (Retinopathy): Diabetes can damage the blood vessels in the retina, potentially leading to vision loss and even blindness.
-
Foot Damage: Poor blood flow and nerve damage can lead to foot sores, infections, and in severe cases, amputation.
-
Hearing Impairment: Diabetes may contribute to hearing loss.
-
Skin Conditions: Individuals with diabetes are more susceptible to bacterial and fungal infections of the skin.
-
Alzheimer's Disease: Research suggests a link between Type 2 Diabetes and an increased risk of Alzheimer's disease.
Regular monitoring of blood sugar levels and adherence to a treatment plan are crucial to preventing or delaying these serious complications.
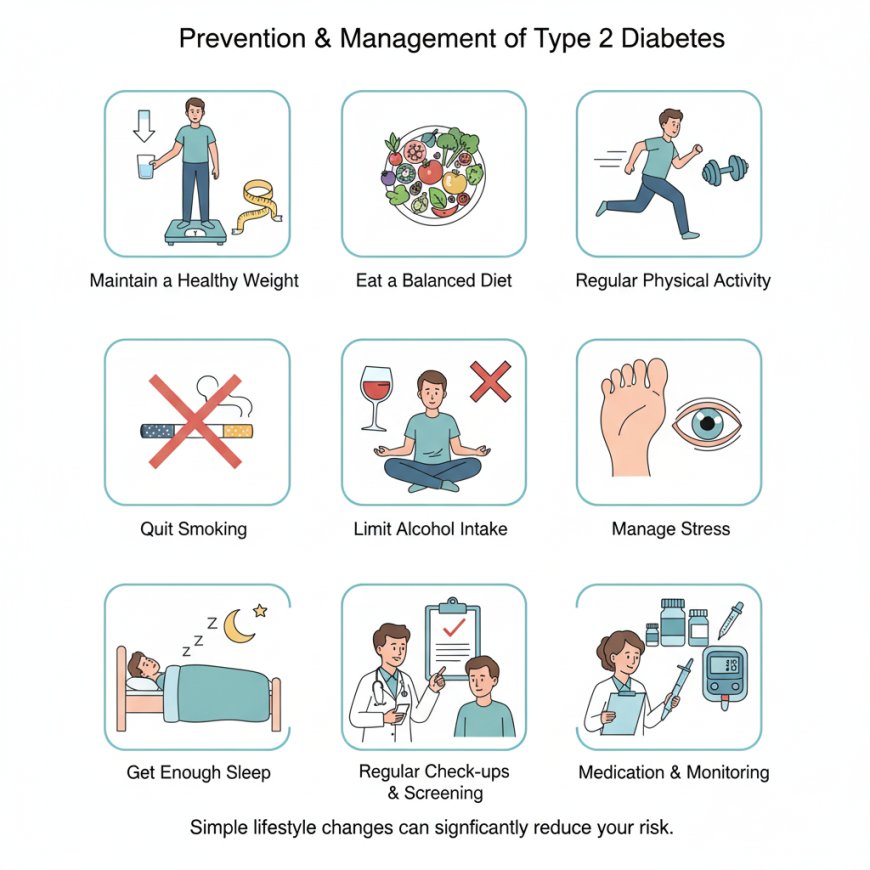
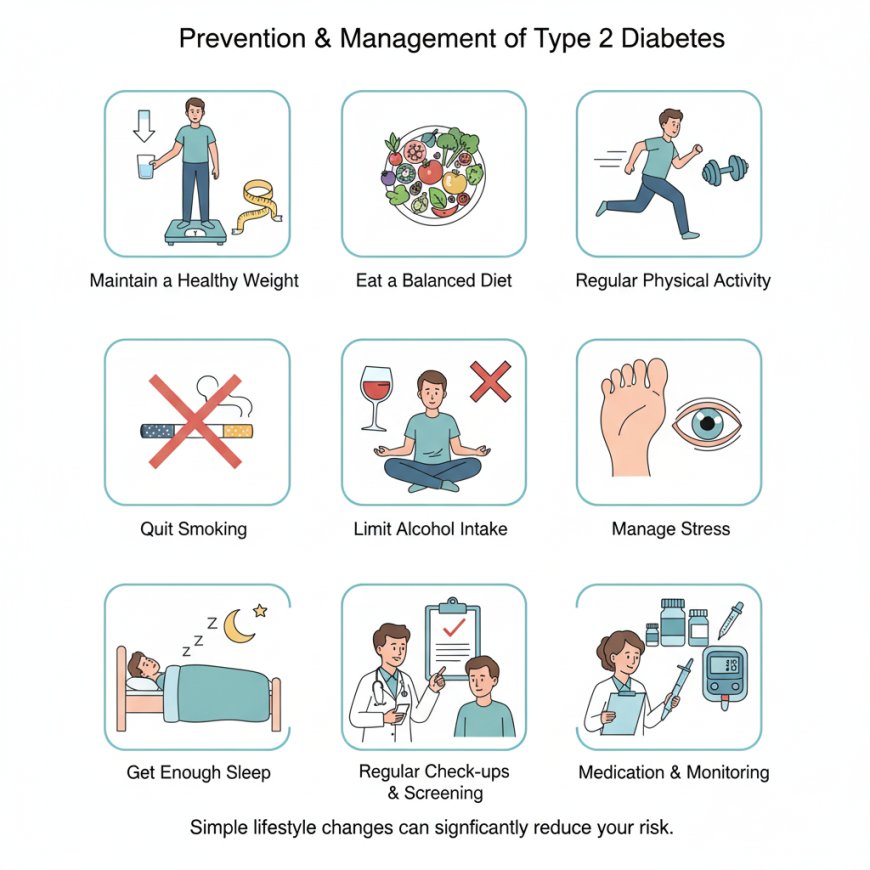
Taking Control: Prevention of Type 2 Diabetes
The good news is that Type 2 Diabetes is largely preventable, especially if you are at risk. Lifestyle modifications play a significant role in reducing your chances of developing the condition.
Key Prevention Strategies Include:
-
Maintain a Healthy Weight: Losing even a modest amount of weight can significantly improve insulin sensitivity.
-
Eat a Balanced Diet: Focus on whole, unprocessed foods. Incorporate plenty of fruits, vegetables, whole grains, and lean proteins. Limit sugary drinks, refined carbohydrates, and unhealthy fats.
-
Engage in Regular Physical Activity: Aim for at least 150 minutes of moderate-intensity aerobic activity per week, along with muscle-strengthening activities at least two days a week. Exercise helps lower blood sugar and improve insulin sensitivity.
-
Quit Smoking: Smoking increases the risk of diabetes and its complications.
-
Limit Alcohol Intake: Excessive alcohol consumption can lead to weight gain and affect blood sugar levels.
-
Manage Stress: Chronic stress can affect blood sugar levels. Find healthy ways to cope with stress, such as meditation, yoga, or hobbies.
-
Get Enough Sleep: Insufficient sleep can negatively impact insulin sensitivity. Aim for 7-9 hours of quality sleep per night.
-
Regular Check-ups: If you have risk factors for diabetes (e.g., family history, obesity, gestational diabetes), regular screenings can help detect the condition early.
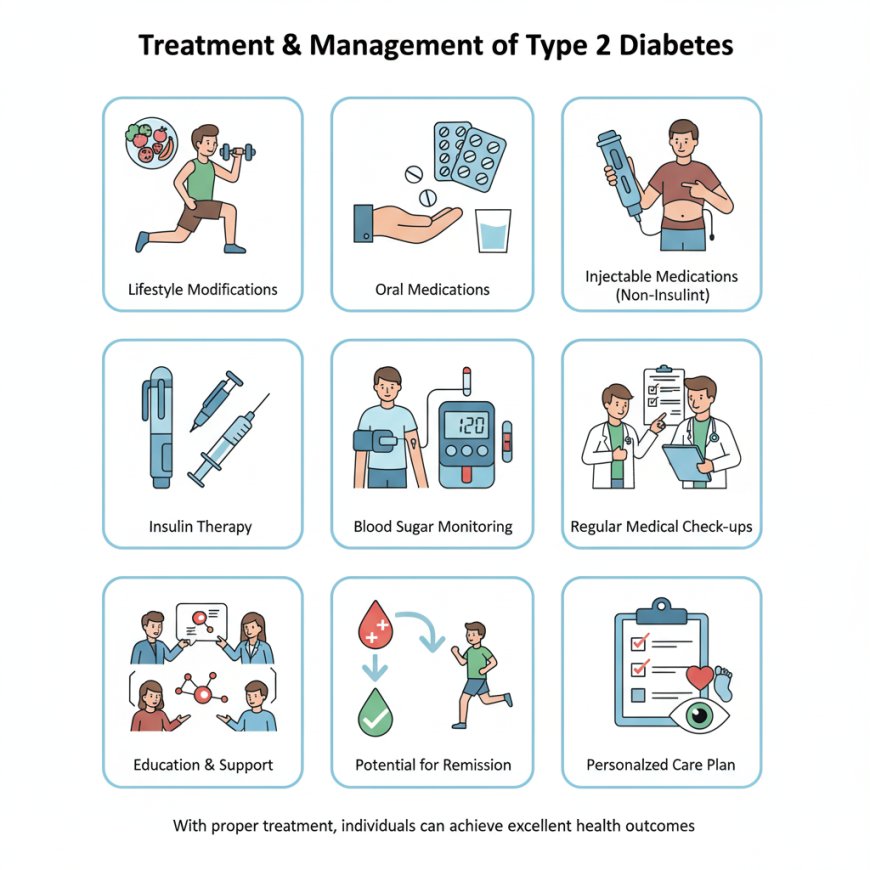
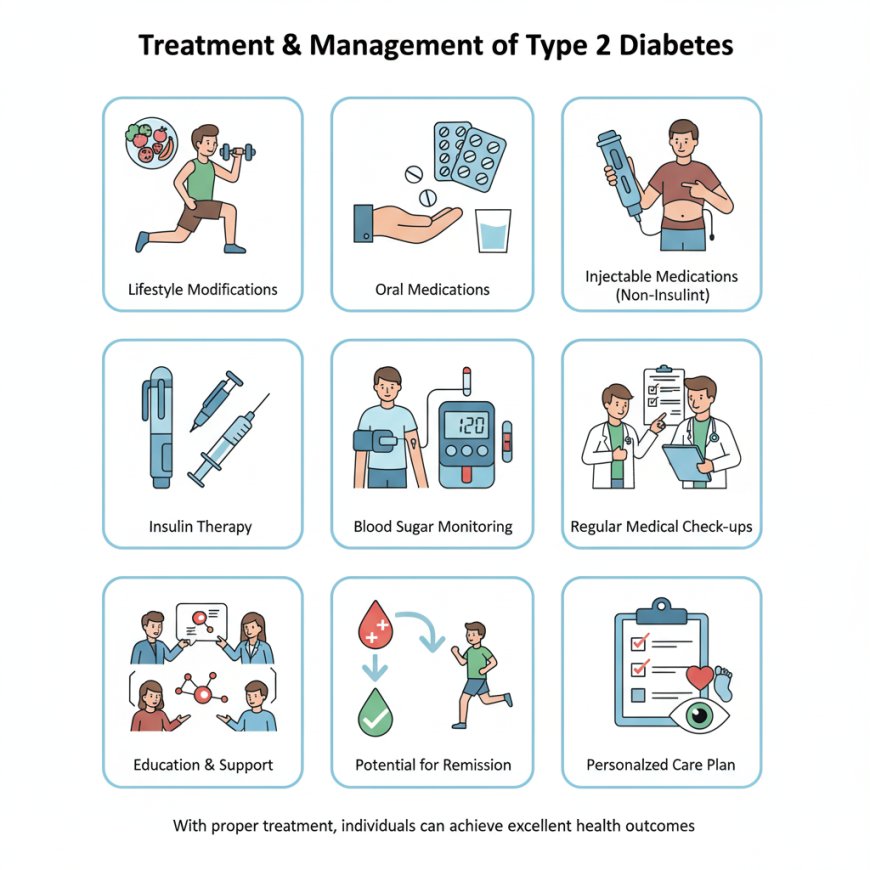
Managing Type 2 Diabetes: Current Approaches to Treatment
While there is currently no "cure" for Type 2 Diabetes in the sense of eradicating it entirely, it is a highly manageable condition. With proper treatment and lifestyle adjustments, many individuals can achieve excellent blood sugar control and prevent or delay complications.
Treatment Strategies Often Include:
-
Lifestyle Modifications: As mentioned in prevention, diet and exercise are fundamental to managing Type 2 Diabetes. A registered dietitian can help create a personalized meal plan.
-
Oral Medications: Various oral medications are available to help lower blood sugar in different ways, such as by increasing insulin production, improving insulin sensitivity, or reducing glucose absorption.
-
Injectable Medications (Non-Insulin): Some injectable medications, like GLP-1 receptor agonists, can help lower blood sugar and promote weight loss.
-
Insulin Therapy: If the pancreas is no longer producing enough insulin, or if other medications are not sufficient, insulin injections may be necessary.
-
Blood Sugar Monitoring: Regularly checking blood sugar levels, either with a traditional blood glucose meter or a continuous glucose monitor (CGM), is essential for understanding how food, activity, and medication affect your body.
-
Regular Medical Check-ups: Consistent visits with your healthcare team (endocrinologist, primary care physician, ophthalmologist, podiatrist, etc.) are vital for monitoring your condition and addressing any potential complications.
-
Education and Support: Understanding your condition and having a support system can empower you to make informed decisions and stick to your treatment plan.
In some cases, especially with significant and sustained lifestyle changes, some individuals with Type 2 Diabetes can achieve remission, where blood sugar levels return to normal without medication. However, this still requires ongoing healthy habits and monitoring.
In conclusion, Type 2 Diabetes is a serious but manageable chronic condition. By understanding its symptoms, potential complications, and effective strategies for prevention and management, individuals can take proactive steps towards a healthier life. Early diagnosis, consistent lifestyle modifications, and adherence to a personalized treatment plan are key to living well with Type 2 Diabetes and minimizing its impact on your health.