Arthritis: Symptoms, Causes, Prevention, and Management
Arthritis: Symptoms, Causes, Prevention, and Management

Arthritis is a widespread condition characterized by inflammation of the joints, leading to pain, stiffness, and sometimes swelling. It's not a single disease but rather an umbrella term encompassing over 100 different types, each with its own unique causes, symptoms, and treatment approaches. Affecting millions worldwide, arthritis can significantly impact a person's quality of life, making everyday activities challenging.
Common Symptoms of Arthritis
While the specific symptoms can vary depending on the type of arthritis, several common indicators often point to the condition:
-
Joint Pain: This is the most prevalent symptom, often described as a dull ache, sharp pain, or throbbing sensation in or around the joint.
-
Stiffness: Joints may feel stiff, especially in the morning or after periods of inactivity. This stiffness can make it difficult to move the affected joint.
-
Swelling: Some types of arthritis cause visible swelling around the affected joints, which may feel warm to the touch.
-
Reduced Range of Motion: The ability to move a joint through its full range of motion may be limited, making certain movements painful or impossible.
-
Redness of the Skin: The skin over the affected joint may appear red.
-
Fatigue: Generalized fatigue can be a significant symptom, particularly in inflammatory types of arthritis.

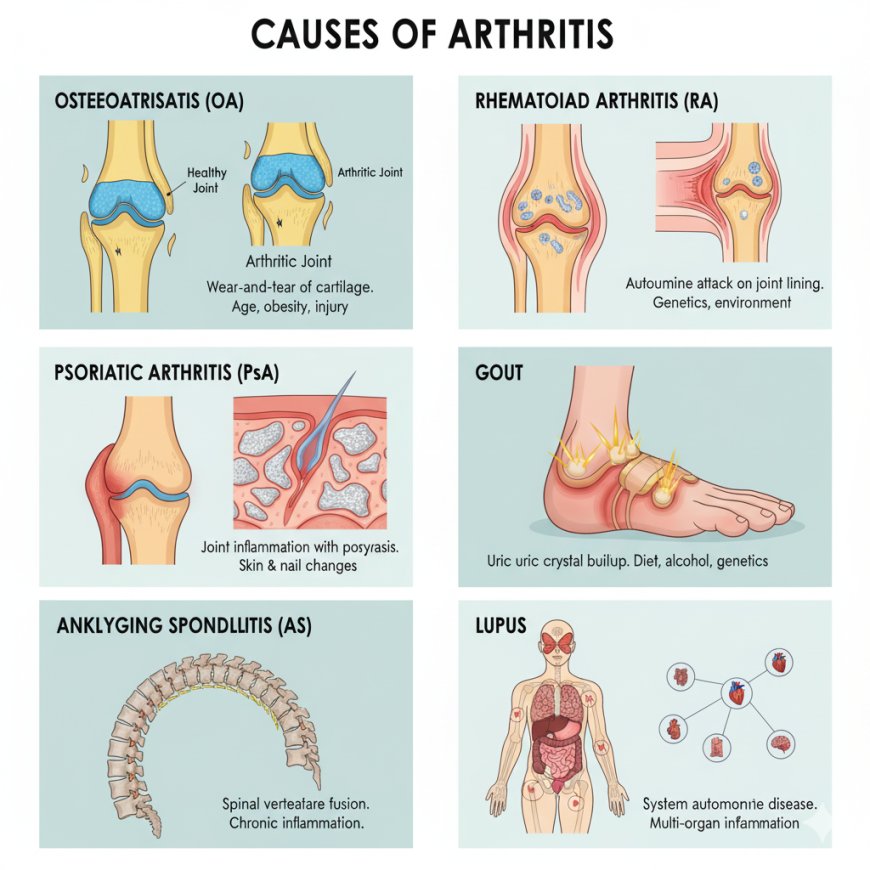
Causes of Arthritis
The causes of arthritis are diverse and depend heavily on the specific type. Here are some of the most common categories:
-
Osteoarthritis (OA): Often referred to as "wear-and-tear" arthritis, OA is the most common form. It occurs when the cartilage that cushions the ends of bones wears down over time, leading to bones rubbing directly against each other. Factors like age, obesity, joint injury, and genetics increase the risk.
-
Rheumatoid Arthritis (RA): This is an autoimmune disease where the body's immune system mistakenly attacks the lining of the joints (synovium), leading to inflammation, pain, and eventually joint damage. Genetics and environmental factors are believed to play a role.
-
Psoriatic Arthritis (PsA): Affecting some people with psoriasis, a skin condition, PsA causes joint inflammation, often accompanied by skin and nail changes.
-
Gout: Caused by the buildup of uric acid crystals in the joints, typically affecting the big toe first. Diet, alcohol consumption, and certain medications can contribute to gout.
-
Ankylosing Spondylitis (AS): Primarily affecting the spine, AS is an inflammatory disease that can lead to fusion of the vertebrae, resulting in a hunched posture.
-
Lupus: Another autoimmune disease, lupus can cause joint pain and inflammation, along with a wide range of other symptoms affecting various organs.
Prevention and Risk Reduction
While not all types of arthritis can be completely prevented, several strategies can help reduce your risk and manage symptoms:
-
Maintain a Healthy Weight: Excess weight puts added stress on weight-bearing joints like knees and hips, increasing the risk of osteoarthritis.
-
Stay Active: Regular, low-impact exercise (like swimming, cycling, or walking) strengthens muscles around joints, improves flexibility, and helps maintain cartilage health.
-
Protect Your Joints: Avoid activities that put excessive strain on your joints. Use proper lifting techniques and protective gear during sports.
-
Eat a Balanced Diet: An anti-inflammatory diet rich in fruits, vegetables, whole grains, and omega-3 fatty acids can help reduce inflammation throughout the body.
-
Quit Smoking: Smoking is a known risk factor for rheumatoid arthritis and can worsen symptoms in other forms of inflammatory arthritis.
-
Limit Alcohol (especially for gout): Excessive alcohol consumption can trigger gout attacks.
-
Manage Other Health Conditions: Effectively managing conditions like diabetes, which can impact joint health, is important.
-
Regular Check-ups: Early diagnosis and intervention can significantly impact the progression and severity of certain types of arthritis.
-

Management and Treatment (Cure)
Currently, there is no "cure" for most types of arthritis, meaning the underlying condition cannot be reversed. However, significant advancements in medical treatments and management strategies allow many people to effectively control symptoms, slow disease progression, and maintain a good quality of life. Treatment approaches are highly individualized and often involve a combination of therapies:
-
Medications:
-
Pain Relievers: Over-the-counter options like acetaminophen or NSAIDs (ibuprofen, naproxen) can help with pain.
-
Disease-Modifying Antirheumatic Drugs (DMARDs): Used for inflammatory arthritis (like RA, PsA) to slow disease progression and prevent joint damage.
-
Biologics: A newer class of DMARDs that target specific parts of the immune system.
-
Corticosteroids: Powerful anti-inflammatory drugs used for short-term relief during flare-ups.
-
Uric Acid Reducers: For gout, these medications help lower uric acid levels.
-
-
Physical and Occupational Therapy: Therapists can teach exercises to improve strength, flexibility, and range of motion. Occupational therapists can help adapt daily tasks to minimize joint stress.
-
Lifestyle Modifications:
-
Exercise: Tailored exercise programs are crucial for maintaining joint function.
-
Weight Management: Essential for reducing stress on joints.
-
Heat and Cold Therapy: Can provide temporary relief from pain and stiffness.
-
Assistive Devices: Can help with daily tasks and reduce joint strain.
-
-
Surgery: In severe cases, when other treatments fail and joint damage is extensive, surgery may be an option. This can include joint repair, joint fusion, or total joint replacement (e.g., knee or hip replacement).